Systemic Risk Factor Management
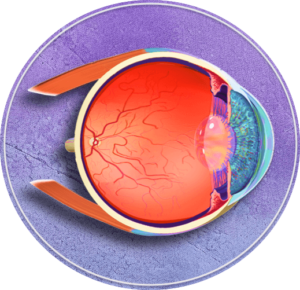
Although treatments such as laser photocoagulation and intraocular injections of medication (including anti-vascular endothelial growth factor [VEGF] or corticosteroids) can decrease the severity of diabetic retinopathy (DR) and lower the risk of vision complications, managing systemic risk factors is also of vital importance.1 Remarkably, managing risk factors can prevent the development as well as progression of DR.2-8 Identifying and managing these systemic factors is key to improving outcomes for affected patients, as DR can result in visual impairment and blindness in its most severe stages, with a deleterious impact on quality of life.2,9
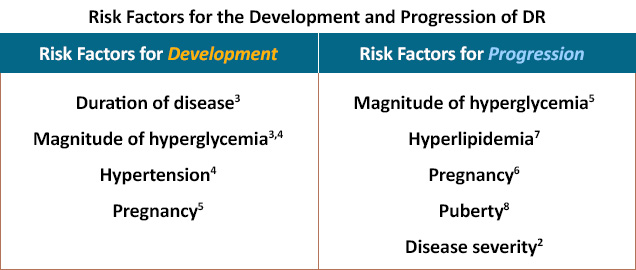
Two key targets of preventive management include glycemic and blood pressure control.1,2,10 The risk for developing DR increases with the duration of diabetes (both type 1 and type 2); however, after retinopathy is present, duration of diabetes is overshadowed by the degree of hyperglycemia.10 Therefore, the importance of glycemic control cannot be understated, as even a 1% reduction in HbA1c can curb the risk of DR progression by 50%.11-13 In general, the goal for HbA1c control is 7% or lower, though this target may need to be adjusted for older patients due to increased morbidity with HbA1c levels below 7%.1,2,10
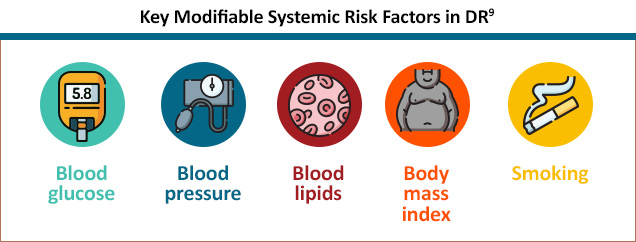
Control of hypertension may also be beneficial; although evidence for intensive management is inconclusive, elevated blood pressure has been associated as a predictor of development/progression of DR.10,14 Additionally, optimizing control of other comorbid conditions, including dyslipidemia, overweight or obesity, renal disease, coronary artery disease, and neuropathy, may also prevent the progression and resultant complications of DR.1,9,10 Patients should also be encouraged to adhere to treatment for comorbidities as part of a comprehensive approach to DR management, which can help preserve vision health in diabetes.7
References
- Boyd K; American Academy of Ophthalmology. Diabetic Retinopathy: Causes, Symptoms, Treatment. October 27, 2022. https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
- Wong TY, Sun J, Kawasaki R, et al. Guidelines on Diabetic Eye Care: The International Council of Ophthalmology Recommendations for Screening, Follow-up, Referral, and Treatment Based on Resource Settings. Ophthalmology. 2018;125:1608-1622.
- Ferris FL 3rd, Nathan DM. Preventing diabetic retinopathy progression. Ophthalmology. 2016;123:1840-1842.
- Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcome: Updated systematic review and meta-analysis. Lancet. 2016;387:435-443.
- Chew EY, Mills JL, Metzger BE, et al. Metabolic control and progression of retinopathy. The Diabetes in Early Pregnancy Study. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Diabetes Care. 1995;18:631-637.
- Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group. Diabetes Care. 2000;23:1084-1091.
- Shi R, Zhao L, Wang F, et al. Effects of lipid-lowering agents on diabetic retinopathy: A meta-analysis and systematic review. Int J Ophthalmol. 2018;11:287-295.
- Lueder GT, Silverstein J. American Academy of Pediatrics Section on Ophthalmology and Section on Endocrinology. Screening for retinopathy in the pediatric patient with type 1 diabetes mellitus. Pediatrics. 2005;116:270-273.
- Risk factors and diabetic retinopathy progression. FutureLearn. https://www.futurelearn.com/info/courses/diabetic-eye-disease/0/steps/47628
- Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020;127:P66-P145.
- Diabetic Retinopathy. National Institutes of Health. National Eye Institute. Last updated July 8, 2022. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) group. Lancet. 1998;352:837-853.
- Cardoso CRL, Leite NC, Dib E, Salles GF. Predictors of development and progression of retinopathy in patients with type 2 diabetes: Importance of blood pressure parameters. Sci Rep. 2017;7:4867.
All URL’s accessed December 7, 2022.